In Britain, every nurse is on grade. The grade depends on experience and skill, and each grade has different responsibilities and pay. On the bottom grades are unqualified auxiliary nurses who do the routine work on hospital wards. On the top grades are nursing officer, who are usually administrators.
Auxiliary nurses are on the bottom grades, but student nurses get the lowest pay. However, student don't stay at the bottom of the scale forever. When they qualify, they start working on a middle grade. As they get experience, they can get promotion and move up the ranks to become staff nurse, then sister (charge nurse if a man), and perhaps eventually nursing officer.
Many Nurse work shift, and often they work overtime to earn more money. After basic training, many nurses choose to do further study and become specialists. Nurses can specialize in many different fields, there are triage nurses working in Casualty, and Psychiatric nurses who treat the mentally ill. There are health visitors who visit patients in their own home, practice nurses working in GPs' surgeries, and midwives who deliver babies.
Many of them say they don't get enough pay and respect for the work they do. They say that the work is physically and mentally hard, that they work long hours and get very tired. But they also say that there are many great rewards which have nothing to do with money.
Nursing Care Plan for Obsessive-Compulsive Disorder
The obsession and compulsion can cause intense stress and impairement of functioning. Fear of losing control, fear of losing the self esteem, overly conscientious, perfectionistic, have trouble to being spontaneously and filled with self-doubt are common experiences by client. Frequently the client will use defence mechanisms of denial, reaction formation, isolation and undoing.
Read more...!
Management Nursing Care Plans @ 12:48 AM,
,
![]()
Nursing Care Plan for Bipolar Disorder
bipolar I, in which depressive episode alternate with full manic episodes.
bipolar II, characterized by recurrent depressive episodes and occasional with manic episodes.
Assesment findings for bipolar disorder
- During periods of mania;
- bizarre and eccentric appereance
- difficulty concentration, flight of idea, delusion of grandeur and impaired judgment
- decreased sleep
- motor agitation
- feeling of grandiosity
- rapid jumbled speech
- deteriorated physical appearance
- euphoria, hostility
- dry mouth, tremors, tachycardia, labored respirations
- inflated sense of self-worth
- increased social contact
- increased libido
- lack of inhibition, recklessness
- anorexia and weight loss, constipation
- altered sleep patterns
- decreased alertness, difficulty thinking logically
- confusion and indecisiveness
- guilt, helplessness, sadness and crying
- amenorrhea
- lack of motivation, low self-esteem, poor self-hygiene
- irritability, pessimism
- impotence and lack of interest in sex
- inability to experience pleasure
During periods of depression;

Treatment for bipolar disorder
- Anticonvulsant agent : carbamazepine (tegretol), divalproex sodium.
- Selective serotonin reuptake inhibitor : paroxetine
- Antimanic agent : lithium carbonate(eskalith), lithium citrate(cibalith-S)
- Individual therapy and family therapy
- Electroconvulsive therapy if drug therapy fails
- Disturbed thought processes
- Impaired social interaction
- Risk for injury
- Disturbed sleep pattern
- demonstrate a stable mood and practice self-care activities
- control thought processes
- demonstrate a normal sleep pattern
- interact adequately with others
- not harm himself
- During manic phase;
- decrease environmental stimuli, to promote relaxation and enable to sleep
- monitor drug level, especially lithium
- ensure safe environment to protect the client
- define and explain acceptable behaviors and then set limits
- if a mood swing to depression, implement suicide precaution for client
- channel the client's energy in one direction and pace activities, to decrease client's energy expenditure, prevent overstimulation and have soothing effect
- assess the risk of suicide and formulate a safety contract with client
- assess the level and intensity if client's depression to obtain baseline information
- ensure a safe environment to client to protect from self-inflicted harm
- encourage the client to identify current problems and stressors, so that can begin with therapeutic treatment
- select activities that ensure success and accomplishment to increase self esteem
- spend time with the client, evens if he's too depressed to talk, in order to enhance therapeutic relationship
- help the client to modify negative expectations and think more positively
- promote opportunities for increased involvement in activities through a structures and daily program
- observe the client for medication compliance and adverse effect
During depressive phase;
- doesn't harm himself or others
- maintains adequate on medication and nutrition
- sleeps throught the night
- expresses understanding of the illness and states how to obtain assistance or support from others
- engages in goal-directed activity and no longer exhibits disturbed thinking
Read more...!
Management Nursing Care Plans @ 2:05 AM,
,
![]()
Nursing Care Plan for Retinal Detachment
Assessment findings of retinal
detachment :
- Painless change in vision (floaters caused by blood cells in the vitreous and flashes of light as the vitreous humor pulls on the retina).
- Photopsia ( recurrent flashes of light).
- Blurred vision worsening as detachment increases.
- with progression of detachment, painless vision loss that may be described as veil, curtain or cobweb that eliminates part of the visual field.
- Indirect opthalmoscopy shows retinal tear or detachment.
- Slit-lamp examination reveals retinal tear or detachment.
- Ultrasound shows retinal tear or detachment in presence of cataract.
- Complete bed rest and restriction of eye movement to prevent further detachment.
- Laser theraphy, if there's a hole in the posterior portion of the retina
- Scleral buckling to reattach the retina, It is a surgical procedure, which a silicone band or sponge is sewn around the eyeball a little behind the visible portion or the eye. Exactly locates the hole and places the band and tightens it creating a buckle effect and then the outer coats of the eye are indented and in this way the hole in the retina approximates the outer scleral coat.
- Pneumatic Retinopexy, It is a short simple procedure, where a fixed amount of air is injected in the posterior part of the eye, which the air acts as an internal tamponade that helping to push and approximate the tear with the outer coat of the eye ball. Following the tear is sealed with cryo or laser therapy. Post-operatively the patient is advised rest in a specified position, in order to facilitate the air bubble to push the desired area of the retina with the tear against the sclera.
- Sub-retinal fluid drain : make seep the fluid out through the hole behind the retina that can be drained with a small slit made in the outer coats of the eye to flatten the retina. This procedure is usually done along with sclera bucking to flatten the retina.
- Vitrectomy: The procedure involves cutting and removal of the vitreous gel along with removal of all the fibrous tissue causing traction (pull) on the retina and detaching it, or sometimes the space is replaced with gas or silicon oil. ussually the procedure is done with the help of micro instruments and a fiberoptic light source. The procedure is combined with sclera buckling.
- Cyropexy, if there's a hole in the peripheral retina.
Nursing diagnoses for Retinal Detachment :
- Disturbed sensory perception (visual).
- Anxiety.
- Risk for injury.
- The client will remain free from injury.
- The client will be free from permanent visual impairment.
- The client will understand the treatment options.
- Asses visual status and functional vision in the unaffected eye to determine self care needs.
- Prepare the client for surgery by explaining possible surgical interventions and technique to alleviate some of the client's anxiety.
- Discourage straining during defecation, bending down and hard coughing, sneezing or vomiting to avoid activities that increase intraocular pressure.
- Assist with ambulation, as needed, to help the client remain independent.
- Approach the clients from the unaffected side to avoid startling him.
- Provide assistance with activities of daily living to minimize frustation adn strain.
- Orient the client to his environment to reduce the risk of injury.
- Posoperatively instruct the client to lie on his back or on his unoperated side to reduce intraocular pressure in the affected area.
- The client's vision is restored.
- The client will remains free from injury.
- The client will understands all discharge instructions.
Read more...!
Management Nursing Care Plans @ 12:03 AM,
,
![]()
Nursing Care Plan for Chronic Obstructive Pulmonary Disease (COPD)
There are two main forms of COPD :
- Chronic obsturctive bronchitis, a productive cough that persisting for 3 months of the year for at least 2 consecutive years, causes inflamed airways that lead to increased mucus production and bronchospasms. Mucus plugs entrap air and result in alveolar hyperventilation. Patient will have severe hypoxemia and polycythemia, with hematrocit values from 50 % to 55 %.
- Emphysema, characterized by enlargment of the alveoli distal to the terminal bronchioles, leads to alveolar wall destruction. obstructed expiratory airflow and irreversible loss of the lung elasticity. It is causes less hypoxemia and hematrocit values commonly normal.
- Allergens.
- Smoking.
- Alpha-1 antitrypsin deficiency.
- Chronic respiratory tract infection.
- Airborne irritants and pollutants, like certain gases or fume in the workplace and using cooking fire without proper ventilation.
Assesment findings in COPD :
- Anatomic changes (such as barrel chest and clubbing) in late disease.
- Cough (evaluate characther, frequency and time of day).
- Decreased breath sounds, hyperresonant breath sounds on percussion and wheezing.
- Cor pulmonale (right-sided heart failure).
- Prolonged expiration.
- Dyspena.
- Jugular vein distention.
- Peripheral edema.
- Use of accessory muscles.
- Pursed-lip breathing.
- Sputum (amount, color and consistency).
- Use of accessory muscles.
- Risk factors.
- ABG levels show hypercapnia and hypoxemia. Bicarbonate levels may increase to compensate for chronic hypercapnia and the resultant respiratory acidosis.
- Pulmonary function test, especially spirometry, reveal diminished lung function.
- Pulse oximetry may show a decrease in arterial oxygen saturation, which indicates impending hypoxia.
- Complete blood count shows elevated hemoglobin level and hematocrit.
- Chest X-ray provides baselines norms; in late disease, the patient's diaphragms appears flat.
- ECG shows signs of right ventricular hyperthrophy in late disease.
- O2 therapy at 2 to 3 L per minute and transtracheal therapy for home O2 therapy.
- Fluid intake up to 3 L per day if not contraindicated by heart failure.
- Chest physiotherapy, postural drainage and incentive spirometry.
- Diet high in protein, vitamin C. calories and nitrogen. Patients with advanced disease may require a diet thats's low in carbohydrates and higher in fats.
- Antibiotic : infecting organism determines which drugs is used.
- Bronchodilator : aminophylline, terbutaline, theophylline; by nebulizer: albuteral (proventil), ipratropium bromide (atrovent), metaproterenol sulfate (alupent).
- Expectorant : guaifenesin.
- Steroid : hydrocortisone, methylprednisolone sodium succcinate; by nebulizer : beclomethasone, triamcinolone.
- Antacid : aluminum hydroxide gel.
- Diuretic : furosemide (lasix).
- Alpha-1 antitrypsin.
- Vaccine : influenza, pneumovax.
- 1.Ineffective airways clearance.
2.Impaired gas exchange.
3.Fatigue.
4.Chronic low self esteem.
- The client will have an adequately clear airway.
- The client will establish an effective breathing pattern.
- The client will maintain adequate gas exchange.
- The client will remain free from infection.
- The client will understand why he should avoid respiratory irritants.
- Assess respiratory status and ABG and pulse oximetry studies to evaluate oxygenation.
- Administer low-flow oxygen, if indicated, ussually 1 to 2 L per minute in 24 % to 28 % concentrations (Client with emphysema respond only to low oxygen tension, if it too much oxygen reduces the drive to breathe and contributes to respiratory failure)
- Monitor cardiovascular status to detect arrhythmias related to hypoxia or adverse response to medications.
- Monitor and record amount, color and consistency of sputum.
- Encourage the cllient to drink plenty of fluids and weight patient daily to monitor for fluid overload and right -sided heart failure.
- Monitor electrolytes levels, blood counts and drug levels for indications of possible toxic reaction.
- Encourage activity as tolerated to help the client to avoid fatigue.
- Provide chest physiotherapy, including postural drainage and percussion, incentive spirometry and suction as needed- to aide in removal of secretions.
- Administer medications as prescribed to relieve symptoms and prevent complications.
- The patient remain free from respiratory tract infection.
- The patient will regularly practices breathing exercises and his breathing efficiency increases.
- The patient will stop smoking and obtains a job with little or no exposure to respiratory irritants.
Read more...!
Management Nursing Care Plans @ 4:02 AM,
,
![]()
Nursing Care Plan for Reye's Syndrome
Assesment finding for reye's syndrome:
- Stage 1 : lethargy, vomiting and hepatic dysfunction
- Stage 2 : hypervetilation, hyperactive reflexes, delirium and hepatic dysfunction.
- Stage 3 : coma, decorticate rigidity, hyperventilation and hepatic dysfunction.
- Stage 4 : deepening coma, large fixed pupils, decerebrate rigidity and minimal hepatic dysfunction.
- Stage 5 : seizures, flaccidity, loss of deep tendon reflexes and respiratory arrest (death is usually a result of cerebral edema or cardiac arrest).
Diagnostic evaluation for reye's syndrome :
- CSF analysis shows a WBC count less than 10/ul; with coma. there's increased CSF pressure.
- Blood test results show elevated serum ammonia levels; serum fatty acid and lactate levels are also increased.
- Liver biopsy show fatty droplets uniformly distributed throughout cells.
- Liver function studies show aspartate aminotransferase and alanine aminotransferase are elevated twice from normal levels.
- Coagulation studies reveal prolonged PT and PTT.
Treatment for reye's syndrome :
- Endotracheal intubation and mechanical ventilation to control partial pressure of arterial carbon dioxide levels.
- Induced hypothermia.
- Exchange transfusion.
- Decompressive craniotomy.
- Enteral or parenteral nutrition as needed.
- Transfusion of fresh frozen plasma.
Nursing diagnosis for reye's syndrome :
- Ineffective thermoregulation.
- Decreased intracranial adaptive capacity.
- Impaired physical mobility.
- Impaired gas exchange.
- Risk for fluid volume deficit.
- Risk for impaired skin integrity.
Nursing planning and goals for reye's syndrome :
- The patient will maintain adequate ventilation.
- The patient will maintain a normal respiratory status, as evidenced by normal respiratory rate.
- The patient will maintain orientation to environment without evidence of deficit.
- The patient will maintain skin integrity.
- The patient will maintain joint mobility and range of motion.
Nursing implementation for reye's syndrome :
- Monitor vital signs and pulse oximetry to determine oxygenation status.
- Monitor ICP with a subarachnoid screw or other invasive device to closely assess for increased ICP.
- Monitor blood glucose levels to detect hyperglycemia or hypoglycemia and to prevent complications.
- Monitor fluid intake and output to prevent fluid overload.
- Assess cardiac, respiratory and neurologic status to evaluate the effectiveness of interventions and monitor for complications such as seizures.
- Assess pulmonary artery catheter pressures to assess cardiopulmonary status.
- Keep the head of the bed at a 30 degree angle to decrease ICP and promotes venous return.
- Maintain seizures precautions to prevent injury.
- Maintain oxygen therapy, which may include intubation and mechanical ventilation, to promote oxygenation and maintain thermoregulation.
- Administer medications as ordered and monitor for adverse effects to detect complications.
- Administer blood products as necessary to increase oxygen-carrying of blood and to prevent hypovolemia.
- Check for loss of reflexes and signs of flaccidity to determine degree of neurologic involvement.
- Provide a hypothermia blanket as needed and monitor the client's temperature every 15 to 30 minute while the blanket is in use to prevent injury and maintain thermoregulation.
- Provide postoperative craniotomy care in necessary to promote wound healing and to prevent complications.
- Provide good skin and mouth care and perform ROM exercise to prevent alteration in skin integrity and to promote joint motility.
- Be supportive of the family and keep them informed of the patient status to decrease anxiety.
Evaluation for reye's syndrome :
- The patient returns to normal respiratory state without sign of respiratory distress.
- The patient will maintain joint mobility and range of motion as well as skin integrity during hospital course.
- The patient has minimal neurologic complication as ICP decreases, as evidenced by reflexes, LOC and orientation.
- The parent verbalize an understanding of avoiding this syndrome by using nonsalicylate analgesic and antypiretic.
Read more...!
Management Nursing Care Plans @ 2:14 AM,
,
![]()
Nursing Care Plan For Sickle Cell Anemia
Read more...!
Management Nursing Care Plans @ 4:26 AM,
,
![]()
Nursing Care Plan For Depressive Disorder
The common symptoms of depressive disorder are apathy, sadness, hopelessness, helplessness, worthlessness, guilty, sleep disturbance, anger, etc. Sometimes followed by other symptoms like; thoughst of death, fatique, decreased libido, psychomotor agitation, dependency, passiveness, spontanious crying without apparent cause.
Before giving nursing care plan for patient with depressive disorder, there are things should asses, including;
- History of onset of symptoms.
- The presence of non-mood psychiatric disorder.
- Interpersonal and coping abilities.
- Level of stressor.
- Presence and or level of suicidal ideation.
- Presence of comorbid subtance, alcohol and medication.
- Patient resources and social support systems.
- Physical examination to rule out possibility of the presence of medical ilness.
Key Nursing Interventions for Depressed Patients;
- Accept patients where they are and focus on their strengths.
- Reinforce decision making by patients.
- Never reinforce hallucinations or delusions.
- Respond to anger theraupeutically.
- Spend time with withdrawn patients.
- Make decision for patients that they are not ready to make for them self.
- Involve patients in activities in which they can experience success.
Labels: NCP Depressive Disorder
Read more...!
Management Nursing Care Plans @ 2:59 AM,
,
![]()
Nursing Care Plans Ebook and Software
Most popular of NCP eBook sell on the market are Critical Care Nursing Care Plans, Maternal-Infant Nursing Care Plans, and NCP Guidelines for Individualizing Patient Care. For some countries, they have started using network connection between nursing division (hospital ward or department) especially in the private hospital with International standard. To provide good quality of Nursing Care Plan, They will set their project using Nursing Care Plan Software such as NCP Secure Entry Client Software.

It used information to guide the nurses or midwife by care paths and flow charts system in a clear concise review of the physiological and psychological changes associated with each perinatal period. Nursing care plans procedure start from basic step like emphasizing assessments, interventions and evaluations for normal healthy pregnancies. This eBook is a helpful complement to other maternal-child nursing texts and in nursing practice.
A comprehensive Nursing care plans for the nurses which including of rationales for every intervention. These eBook also contains comprehensive Critical thinking emphasized throughout, promoting thoughtful decision making and better individualization care. It is not only available in the PDF format, but also available in CD-ROM.

The NCP Secure Entry Client proves, how easy it is to use NCP VPN clients. Part of its user friendliness is due to its intuitive GUI. used in connection with IPsec gateways from third party manufacturers - as an alternative to their VPN clients - due to their extensive security and telecommunications performance features.

The NCP Secure Entry Client software has integrated, dynamic personal firewall and it's predestined for deployment in the most remote access projects which no central management of teleworking stations is required.
Labels: Nursing eBook
Read more...!
Management Nursing Care Plans @ 8:04 PM,
,
![]()
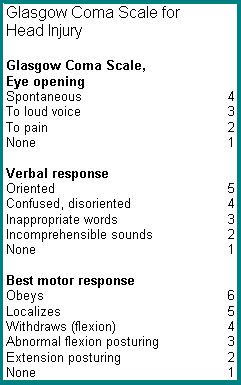
Nursing Care Plan For Acute Head Injury
A. Assessment Findings on Acute Head Injury
Possible causes of acute head injury are assault, automobile accident, blunt trauma, fall and penetrating trauma. The medical team should be perform serious and critical care to handle this cases, So that they can finding correct assessment may happened to the patients such as:
- Disorientation to time, place or person
- Unequal pupil size, loss of pupillary reaction
- Decreased LOC
- Paresthesia
- Otorrhea, rhinorea, frequent swallowing.
B. Diagnostic Evaluation for Acute Head Injury
C. Nursing Diagnose in Acute Head Injury
- Ineffective tissue perfusion (cerebral)
- Risk for Injury
- Decreased intracranial adaptive capacity.
D. Treatment of Acute Head Injury
- Cervical collar (until neck injury is ruled out)
- Craniotomy; surgical incision into te cranium (may be necessary to evacuate a hematoma or evacuate contents to make room for swelling to prevent herniation)
- Oxygen (O2) Therapy; intubation and mechanical ventilation (to provide controlled hyperventilation to decrease elevate ICP)
- Restricted oral intake for 24 to 48 hours
- Ventriculostomy; insertion of a drain into the ventricles (to drain CSF in the presence of hydrocephalus, which may occur as a result of head injury; can also be used to monitor ICP).
E. Drug Therapy Options for Head Injury Cases
- Analgesic; codein phosphate
- Anesthetic; Lidocin (Xylocaine)
- Anticonvulsant; Phenytoin (Dilantin)
- Barbiturate; pentobarbital (Nembutal), if unable to control ICP with diuresis
- Diuretic; mannitol (Osmitrol), furosemide (Lasic) to combat cerebral edema
- Dopamine (Intropin) to maintain cerebral perfusion pressure above 50 mmHg (if blood pressure is low and ICP is elevated)
- Glucocorticoid; dexamethasone (Decadron) to reduce cerebral edema
- Histamin-2 (H2) receptor antagonist such as cimetidine (tagamet), ranitidine (Zantag), famotidine (Pepcid), nizatidine (Axid)
- Mucosal barriel fortifier; sucralfate (Carafate)
- Posterior pituitary : vasopressin (Pitressin) if client develops diabetes insipidus.
F. Planing and Goal on Nursing Care Plan
- The patient will have improved cerebral perfusion
- The patient will have decreased ICP
- The patient will have remain free from injury.
G. Implementation of Nursing Care Plan Procedure
- Assest neurologic and respiratory status to monitor for sign of increased ICP and respiratory distress
- Monitor and record vital sign and intake and output, hemodynamic variables, ICP, cerebral perfusion pressure, specific gravity, laboratory studies, and pulse oximetry to detect early sign of compromise.
- Observe for sign of increasing ICP to avoid treatment delay and prevent neurologic compromise
- Assess for CSF leak as evidenced by otorhea or rinorrhea. CSF leak could leave the patient at risk for infection
- Assess for pain. Pain may cause anxiety and increase ICP
- Check cough and gag reflex to prevent aspiration
- Check for sign of diabetes insipidus (low urine specific gravity, high urine output) to maintain hydration
- Administer I.V fluids to maintain hydration
- Administer Oxygen to maintain position and patency of endotracheal tube if present, to maintain airway and hyperventilate the patient and to lower ICP
- Provide suctioning; if patient is able, assist with turning, coughing, and deep breating to prevent pooling of secretions
- Maintain postion, patency and low suction of NGT to prevent vomiting
- Maintain seizure precautions to maintain patient safety
- Administer medication as prescription to decrease ICP and pain
- Allow a rest period between nursing activities to avoid increase in ICP
- Encourage the patient to express feeling about changes in body image ot allay anxiety
- Provide appropriate sensory input and stimuli with frequent reorientation to foster awarness of the environtment
- Provide means of communication, such as a communcation board to prevent anxiety
- Provide eye, skin, and mouth care to prevent tissue damage
- Turn the patient every 2 hours or maintain in a rotating bed if condition allows to prevent skin breakdown.
H. Evaluation of Goals in the Nursing Care Plan
- The patient has improved LOC
- The patient hasdoest not exhibit signs of increased ICP
- The patient hasremains free from injury
Labels: NCP Head Injury
Read more...!
Management Nursing Care Plans @ 10:29 PM,
,
![]()
Nursing Care Plan For Acute Renal Failure
Acute renal failure (ARF) or Acute Kidney Injury (AKI) is a rapid loss (breakdown or decrease) of renal function due to damage to the kidneys, resulting in retention of nitrogenous (urea and creatinine) and non-nitrogenous waste products that are normally excreted by the kidney.
Acute Renal Failure (ARF) is classified as :
- Pre Renal; occurs as a result of renal hypoperfusion which usually responds well to rehydration, or result from condition that diminish blood flow to the kidney.
- Intra Renal; result from damage to the kidneys, usually from acute tubular necrosis. In critically ill patients other insults such as infection, hypoxia, drugs etc, may convert a simple problem of poor perfusion into one of acute tubular necrosis where there is structural damage to the renal parenchyma. The patient may not die from renal failure although this may be present at the time of death. There is a high mortality in patients who develop ARF in the context of other severe illness.
- Post Renal (obstructive); result from bilateral obstruction of urine flow. The most common cause of obstructive uropathy in men is prostate.
The possible causes of acute renal failure are Acute glomerulonephritis, Acute tubular necrosis, Anaphylaxis, Benign prostatic hyperplasia, Blood transfusion reaction, Burns, Cardiopulmonary bypass, Collagen disease, Congenital deformity, Dehydration, Diabetes Mellitus, Heart failure, Cardiogenic shock, Endocarditis, Malignant hypertension, Hemorrhage, Infection (pyelonephritis and septicemia), Neprotoxins (antibiotics, X-ray dyes, pesticides and anesthetic) and Thrombi or emboli.
Nursing care plan (NCP) or nursing intervention for the patients who diagnosed as acute renal failure during admitted on the hospital should be complete, comprehensive monitor and quick action in order to improve of patient's condition.
A. Assessment Findings on Acute Renal Failure
During assessment, the nurses may find some sign and symptom of acute renal failure. There are many complain from patient related to his/her condition such as ; Anorexia, Nausea, Vomiting, Costovertebral plain, Headache, diarrhea or constipation, Irritability, Restlessness, Lethargy, Drowsiness, Stupor, Coma, Pallor, Ecchymosis, Stomatitis, Thick tenaciouse sputum, Urine output less than 400 ml/day for 1 to 2 weeks and then followed by diuresis (3 to 5 L/day) for 2 to 3 weeks, Weight gain.
B. Diagnostic Evaluation for Acute Renal Failure
- Arterial blood gas (ABG) analysis shows metabolic acidosis.
- Blood chemistry shows increased potassium, phosphorus, magnesium, blood urea nitrogen (BUN) creatinine, and uric acid levels. Also decreased of calcium, carbon dioxide, and sodium levels.
- Creatinine clearance is low
- Excretory urography shows decreased renal perfusion and function.
- Glomerular filtration rate (GFR) is 20 - 40 ml/minute (renal insufficiency), 10 - 20 ml/minute (renal failure), or less than 10 ml/minute (end-stage renal disease).
- Hematology shows decreased hemoglobin (Hb) level, hematocrit (HCT), and erythrocytes. Also increase of prothrombin time (PT) and partial thromboplastin time (PTT).
- Urine chemistry shows albuminuria, proteinuria, increase sodium levels {casts, red blood cells (RBCs), and white blood cells (WBCs)}, and urine specific gravity greater than 1.025 which continue fixed at less than 1.010.
C. Nursing Diagnose (Problems) in Acute Renal Failure
- Ineffective tissue perfusion (renal)
- Excess fluid volume
- Risk for infection
- Risk for deficient fluid volume.
D. Treatment of Acute Renal Failure
- Continuous arteriovenous hemofiltration
- Low protein, increased carbohydrate, moderate fat, and moderate calorie dietwith potassium, sodium and phosphorus intake regulated according to serum levels
- Peritoneal dialysis or hemodialysis
- Fluid intake restricted to the amount needed to replace fluid loss.
- Transfusion therapy with packed RBCs administered over 1 to 3 hours as tolerated.
E. There are Many of Drug Therapy Options
- Alkalinizing agent ; sodium bicarbonate
- Antacid ; aluminum hydroxide (AlternaGEL)
- Antibiotic ; cefazolin (Ancef)
- Anticonvulsant ; phenytoin (Dilantin)
- Antiemetic ; prochlorperazine (Compazine)
- Antipyretic ; acetaminophen (Tylenol)
- Beta-adrenergic blocker ; dopamine (Intropin) initially to improve renal perfusion
- Cation exchange resin ; sodium polystyrene sulfonate (Kayexalate)
- Diuretic ; furosemide (Lasix) , metolazone (Zaroxolyn)
F. Planing and Goal of Nursing Care Plane
- The client will have normal fluid and electrolyte levels
- The client will experience no preventable complication
- The client will understand the means by which His/Her family members will implement health teaching after discharge.
G. Nursing Intervention for Acute Renal Failure
To the nursing intervention, the nurses should be have good knowledge to decide which phase of his/her patient related to the acute renal failure. Base on that information, bellow are some nursing intervention they can do to the patient with acute renal failure :
* Oliguric-anuric phase ; In this phase, the client's urine output falls bellow 400 ml/day. With resultant electrolyte imbalance, metabolic acidosis, and retention of nitrogenouse wastes from non functioning nephrons. This pahse may last up to 14 days. The Nurses should be follow these steps :
- Maintain the client on complete bed rest, organize care to provide long rest periods. Activity increase the rate of metabolism, which increase production of nitrogenouse waste product.
- Implement intervention to prevent infection and the complications of immobility. Because She/He is on bed rest, the client becomes susceptible to the hazards of immobility. Infection is a serious risk and the leading cause of death in client with acute renal failure.
- Observe the client for metabolic acidosis to identify complication of renal failure.Observe the fluid and electrolyte balance hourly.
- Insert an indwelling urinary catheter and measure output and specific gravity hourly. These action allow the nurse to monitor the kidneys, which have the major role in regulating fluid and electolyte balance. High potassium levels can occur.
- Provide only enough fluid intake to replace urine output to avoid an edema caused by excessive fluid intake.
- Monitor the client's diet to provide high carbohydrates, adequate fats, and low protein. If client receives high calories from fat and carbohydrate metabolism, the body doesn't break down protein for energy. Protein is thus available for growth and repair.
- Reduce the client's potassium intake to help prevent elevated potassium levels. Protein catabolism causes potassium release from cells into the serum.
- Observe for the arrhytmias and cardiac arrest to identify complications of high serum potassium.
- Provide frequent oral hygiene to avoid tissue irritation and sometime ulcer formation caused by urea and other acid waste products excreted through the skin and mucous membranes.
- Provide the client with hard candy and chewing gum to stimulate saliva flow and decrease thirst.
- Maintain skin care with cool water to relive pruritus and remove uremic frost (white crystal formed on skin from excretion of urea).
- Administer stool softeners to prevent colon irritation from high levels urea and organic acids.
- Provide emotional reassurance to the client and family members to help decrease anxiety levels caused by the fact that the client has an acute illness with unknown prognosis.
- Explain treatments and progress to the client to help reduce anxiety.
- Provide hemodialysis or peritoneal dialysis as ordered.
* Early diuretic phase ; During early diuretic phase, which last about 10 days, the client excretes a large volume (over 3,0000 ml/day) of very dilute urine. The glomeruli are beginning to function effectively, but tubules aren't, and the client still experiences electrolyte imbalance, retention of nitrogenous waste product and metabolism acidosis. The nurse should be do intervention such as ;
- Assess fluid and electrolyte balance to identify continued fluid and electrolyte imbalance when the renal tubules aren't functioning.
- Assess the emotional status of the client and family members to provide support because the prognosis is still uncertain.
- Continue interventions used during the oliguric phase.
* Late Diuretic phase ; In the late diuretic phase, the client is still excreting more fluid than normal. Urine specific gravity is increasing because the tubules are beginning to function effectively. Fluid, electrolyte and acid-base balances are returning to normal. In this condition, The nurse should do the following steps ;
- Continuing implementations of the early diuretic phase. Allow the client to engage in nonstrenuous activity for brief periods and increase the activity level gradually. Don't let him/her become fatigued which may increase the rate of metabolism and overwork the kidneys.
- Teach the client to prevent infection and to avoid the factors that caused renal failure to help prevent a recurrence.
H. Evaluation of Nursing Intervention
- The client regains fluid and electrolyte balance.
- The client understands the rationale behind activity restriction.
Labels: NCP Renal Disease
Read more...!
Management Nursing Care Plans @ 10:11 PM,
,
![]()
Nursing Care Plan For Heart Failure
Heart Failure also called as Cardiac failure, Congestive Heart Failure (CHF). Heart failure (HF) is a medical condition in which a problem with the structure or function of the heart impairs its ability to supply sufficient blood flow to meet the body's metabolic needs.
Heart failure does not mean that your heart has stopped or is about to stop working. It means that your heart is not able to pump blood the way it should. It should not be confused with cardiac arrest. So, the Nursing Care Plan for Heart Failure cases are little different with others heart problems.
Heart failure can occur on the left-sided or right-sided of the heart. Left-sided heart failure causes mostly pulmonary sign and symptom, such as shortness of breath, dyspnea on exertion and a moist cough. Right-sided heart failure causes systemic sign, such as edema and swelling, jugular vein distention and hepatomegaly.

The possible causes of heart failure are atherosclerosis, cardiac conduction defects, chronic obstructive pulmonary disease, fluid overload, hypertension, MI, pulmonary hypertension, valvular insufficiency, valvular stenosis.
Nursing Care Plan For Heart Failure :
A. Assessment Findings on Heart Failure Cases
- Left-sided heart failure ; Dyspnea, Crackles, Orthopnea, Paroxysmal noctural dyspnea, Tachypnea, Tachycardia, Gallop rhythm (third or S3 and fourth or S4 heart sound), Fatigue, Anxiety, Arrhythmias and Cough.
- Righ-sided heart failure ; Dependent edema, Weight gain, Fatique, Jugular vein distention, Tachycardia, Gallop rhythm (S3 or S4), Nausea, Anorexia, Hepatomegaly and Ascites.
B. Diagnostic Evaluation
- Left-sided heart failure ;
- ABG levels indicate hypoxemia and hypercapnia.
- Blood chemistry test results reveal decreased potassium and sodium levels and increased BUN and creatinine levels.
- Chest X-ray shows increased pulmonary congestion and left ventricular hypertrophy.
- ECG may show left ventricular hypertrophy or acute ST-T wave changes.
- Echocardiography shows increased size of cardiac chambers and decreased wall motion. Hymodinamic monitoring reveals increased PAP and PAWP and decreased cardiac output.
- Righ-sided heart failure ;
- ABG levels indicate hypoxemia.
- Blood chemistry test results show decreased sodium and potassium levels and inc creatinine levels.
- Chest X-ray reveals pulmonary congestion, cardiomegaly, and pleural effusions.
- ECG may show left and right ventricular hypertrophy or acute ST_T wave changes.
- Echo cardiogram shows increased size of chambers and decreased in wall motion.
- Hemodynamic monitoring show increased right atrial pressure, CVP, and right ventricular pressure and also decrease cardiac output.
C. Nursing Diagnoses
- Excess fluid volume
- Activity intolerance
- Ineffective health maintenance
Due to possible cases above, the best treatment are :
- Low-sodium diet and limited intake of fluid
- Intra-aortic balloon pump (IABP)
- Oxygen therapy (possible intubation and mechanical ventilator)
- Left ventricular assist device (for left-seded heart failure)
- Paracentesis (for right-sided heart failure)
- Thoracentesis (for right-sided heart failure)
There are many of drugs therapy option, such as :
- Analgesic (morphine sulfat IV)
- Angiotensin-converting enzyme (ACE) inhibitor; {captropil (capoten), enalapril (vasotec), lisinopril (prinivil)}
- Beta-adrenergic blocker ; {carvedilol (coreg), metoprolol (lopressor)}
- Cardiac glycoside; digoxin (lanoxin)
- Diuretic; {bumetanide (bumex), furosemide (lasix), metolazone (zaroxolyn), spironolactone (aldactone)}
- Inotropic agent; {amrinone lactate (inocor), dobutamine hydrochloride (dobutrex), dopamine hydrochloride (intropin)}
- Nitrate; {isosorbite dinitrete (isordil), nitroglycerin (nitro-bid)}
- Vasodilator; nitroprusside sodium (nitropress)
D. Planing and Goals of Nursing Care
- The clients will understand how to cope with necessary lifestyle changes.
- The client won't develop preventable complication
- The client will will understand how to continue therapy at home.
E. Nursing Intervention For Heart Failure
- Assess cardiovascular status, vital sign and hemodynamic variable to detect signs of reduced cardiac output.
- Assess respiratory status to detect increasing fluid in the lungs and respiratory failure.
- Keep the client in semi-fowler's position to increase chest expansion and improve ventilation.
- Administer medication as prescribed, to enhance cardiac performance and reduce excess fluids.
- Administer oxygen to enhance arterial oxygenation.
- Measure and record intake and output, Intake greater than output may indicated fluid retention.
- Monitor laboratory test result to detect electrolyte imbalances, renal failure, and impaired cardiac circulation.
- Provide suctioning, if necessary assist with turning and encourage coughing and deep breathing to prevent pulmonary complication.
- Restrict oral fluid to avoid worsening the client's condition.
- Weigh the client daily to detect fluid retention. A weight gain of 2lb (0,9 kg) in 1 day or 5 lb (2,3 kg) in 1 week indicates fluid gain.
- Measure and record the client's abdominal girth. An increased in abdominal girht suggests worsening fluid retention and right-sided heart failure.
- Make sure the client maintains a low-sodium diet to reduce fluid accumulation.
- Encourage the client to express feelings, such as a fear of dying to reduce anxiety.

F. Evaluation of Nursing Care on Heart Failure Disease.
- The client accurately describes recommended dietary restriction and medication regimens.
- The client hasn't experienced complication
- The client verbalizes important sign and symptom to report.
Labels: NCP Heart Disease
Read more...!
Management Nursing Care Plans @ 11:24 PM,
,
![]()
Nursing Care Plan For Myocardial Infarction (MI)
Myocardial infarction (MI or AMI for acute myocardial infarction) is the rapid development of myocardial necrosis (die of heart cells) caused by a critical imbalance between oxygen supply and demand of the myocardium.
This is serious medical condition that sometimes called as a heart attack or a coronary thrombosis. The medical team should be take quickly action to give treatment and Nursing Care to prevent complication or die.
With myocardial infarction, reduce blood flow in one of the coronary arteries leads to myocardial ischemia, injury and necrosis. From the ECG result, with a Q-wave MI it's mean that the tissue damage extends through all myocardial layers. Non-Q-wave MI, ussually only the innermost layer is damage.
Possible causes of Myocardial infarction (MI) are : Coronary artery occlusion, Coronary spasm and Coronary stenosis. There are some risk factors to develop of Myocardial infarction such as :
- Aging
- Decrease serum HDL levels
- Diabetes Mellitus
- Drug use, specifically use of amphetamines or cocaine
- Elevated serum Triglyceride, LDL and Cholesterol levels
- Excessive intake of saturated fats, carbohydrates, or salt
- Family history of CAD
- Hypertension
- Obesity
- Post menopausal women
- Sedentary lifestyle
- Smoking
- Stress
Nursing Care Plan For Myocardial Infarction (MI):
Assessment findings on the patient with myocardial infarction are : Dyspnea, Diaphoresis, Arrhythmias, Tachicardia, Anxiety, Pallor, Hypotension, Nausea and vomiting, Elevated temperature. The specific complain from the patient is crushing substernal chest pain (may radiate to the jaw, back and arms) that unrelieved by rest or nitroglycerin (NGT) tablet.
Diagnostic evaluation patient with myocardial infarction:
- ECG show deep, wide @ wave ; elevated or depressed ST segment; and T wave inversion or cardiac arrythmias.
- Blood chemistry test result show increased creatine kinase (CK), lactate dehydrogenase (LD), lipid, and troponin T levels; increased WBC count; positive CK_MB fraction; and flipped LD1.
Nursing diagnoses for patient myocardial infarction (MI) are:
- Chest discomfort (pain) due to an inbalance Oxygen (O2) demand supply
- Potential Arrhythmias related to decrease cardiac output
- Respiratory difficulties (dyspnoea) due to decrease CO
- Anxiety & fear of death related to his condition
- Activity intolerance related to limitations imposed
- Potential for complications of thrombolytic therapy
- Discharge medications, follow up & Health teachings
Planing and goals of nursing care plan;
- The patient won't develop preventable complication
- The patient will understand the necessary treatment and lifestyle changes.
Nursing Intervention for myocardial infarction (MI):
- Monitor ECG result to detect ischemia, injury new or extended infarction, arrhythmia, and conduction defects
- Monitor, record vital signs and hemodynamic variables to monitor response to the therapy and detects complication
- Administer oxygen as prescribe to improve oxygen supply to the heart
- Obtain an ECG reading during acute pain to detect myocardial ischemia, injury or infarction
- Maintain the patient's prescribed diet to reduce fluid retention and cholesterol levels
- Provided postoperative care if necessary to avoid postoperative complications and help the patient achieve a full recovery
- Allay the patient's anxiety because the anxiety increase oxygen demands.
Nursing Evaluation for myocardial infarction (MI):
- The patient explains how and when to take medicine and state reportable adverse reaction
- The patient describes appropriate lifestyle changes to reduce the risk of future cardiac event
- The patient experiences no complication after heart attack (myocardial infarction)
Labels: NCP Heart Disease
Read more...!
Management Nursing Care Plans @ 3:01 AM,
,
![]()
Nursing Care Plan For Hypertension
Hypertension or High blood pressure (HBP) is a medical condition in which the blood pressure is chronically elevated in the arteries or blood vessels. Hypertension is also categorized according to etiology: as primary/essential (approximately 95% of all cases), when it has no identifiable cause; or secondary, which occurs as a result of an identifiable, sometimes correctable, pathologic condition.
1. Hypertension (Blood pressure) of 160/100 mmHg or above
This is definitely high, In this level the patient should be treat with medication to lower it. Otherwise, Persistent hypertension can make serious problem such as strokes, heart attacks, heart failure and arterial aneurysm, and is a leading cause of chronic renal failure.
2. Hypertension (Blood pressure) of 140/90 mmHg to 160/100 mmHg
This level called as 'mild' high blood pressure. For many people the risk from mild high blood pressure is small, and drug treatment is not indicated. Anyway, in this range they will get advised medication to lower it. Hypertension increases with age and is one of the major risk factors in the development of cardiovascular disease.
3. Hypertension (Blood pressure) between 130/80 and 140/90 mmHg
For most people this level is fine, But in some group of people this level is too high for them. Treatment to lower the blood pressure if it is 130/80 mmHg or higher may be considered if some one :
- Have developed a complication of diabetes, especially kidney problems.
- Have had a serious cardiovascular event such as a heart attack, transient ischaemic attack (TIA) or stroke.
- Have certain chronic (ongoing) kidney diseases.

Risk factors to get hypertension are ; Aging, Atherosclerosis, Diet (sodium and caffein), Family history, Obesity, Race (insidence is higher in blacks), Sex (incidence is higher in males older than age 40), Smoking and Strees.
Nursing Care Plan For Hypertension :
The Nurses must collect some data during assessment ; Asymptomatic, Elevated blood pressure, Dizziness, Headache, Left ventricular hypertrophy, Heart failure, Cerebral ischemia, Renal Failure, Papilledema, Vsual disturbance (including blindness).
See the diagnostic evaluation ;
- ECG: Ventricular or atrial hypertrophy, axis deviation, ischemia, and damage patterns may be present. Dysrhythmias; e.g., tachycardia, atrial fibrillation, conduction delays, especially left bundle branch block, frequent premature ventricular contractions (PVCs), may be present. Persistent ST-T segment abnormalities and decreased QRS amplitude may be present.
- Chest x-ray: May show enlarged cardiac shadow, reflecting chamber dilatation/hypertrophy, or changes in blood vessels, reflecting increased pulmonary pressure. Abnormal contour; e.g., bulging of left cardiac border, may suggest ventricular aneurysm.
- Sonograms (echocardiogram, Doppler and transesophageal echocardiogram): May reveal enlarged chamber dimensions, alterations in valvular function/structure, the degrees of ventricular dilation and dysfunction.
- Heart scans: Technetium-99m (99mTc) pyrophosphate scaning (also known as hot spot myocardial imaging and infarct avid imaging): Used to detect recent myocardial infaction and its extent.
- Multigated acquisition (MUGA): Measures cardiac volume during both systole and diastole, measures ejection fraction, and estimates wall motion.
- Exercise or pharmacologic stress myocardial perfusion (e.g., dipyridamole [Persantine] or thallium scan): Evaluates blood flow, determines presence of myocardial ischemia and wall motion abnormalities.
- Positron emission tomography (PET) scan: Sensitive test for evaluation of myocardial ischemia/detecting viable myocardium.
- Cardiac magnetic resonance imaging (MRI): Helps detect congenital heart disease, valvular heart disease, and vascular disorders such as thoracic aneurysm. It also helps detect cardiac tumors and structural anomalies.
- Cardiac catheterization: Abnormal pressures are indicative of and help differentiate right-sided versus left-sided heart failure, as well as valve stenosis or insufficiency. Also assesses patency of coronary arteries. Contrast injected
- into the ventricles reveals abnormal size and ejection fraction/altered contractility. Transvenous endomyocardial biopsy may be useful in some clients to determine the underlying disorder, such as myocarditis or amylodosis.
- BNP (Beta-type natruiretic peptide): Affects cardiac function and vascular tone and renal function. Low levels indicate worsening heart failure.
- Liver enzymes: Elevated in liver congestion/failure.
- Digoxin and other cardiac drug levels: Monitored to determine therapeutic range and correlate expected response with client response.
- Bleeding and clotting times: Determine therapeutic range for anticoagulant therapy and/or identify those at risk for excessive clot formation.
- Electrolytes: May be altered because of fluid shifts/decreased renal function and medications (e.g., diuretics, ACE inhibitors).
- Arterial blood gases (ABGs): Left ventricular failure is characterized by mild respiratory alkalosis (early) or hypoxemia with an increased PCO2 (late).
- BUN/creatinine: Elevated BUN suggests decreased renal perfusion as may occur with HF and/or as a side effect of prescribed medications (e.g., diuretics and ACE inhibitors). Elevation of both BUN and creatinine is indicative of renal failure.
- Serum albumin/transferrin: May be decreased as a result of reduced protein intake or reduced protein synthesis in congested liver.
- Complete blood count (CBC): May reveal anemia (major contributor/exacerbating factor in HF), polycythemia, or dilutional changes indicating water retention. Levels of white blood cells (WBCs) may be elevated, reflecting recent/acute MI, pericarditis, or other inflammatory or infectious states.
- ESR: May be elevated, indicating acute inflammatory reaction (especially if viral infection is cause of HF).
- Thyroid studies: Increased thyroid activity suggests thyroid hyperactivity as precipitator of HF. Hypothroydism can also cause or exacerbate HF.
- Pulse oximetry: Oxygen saturation may be low, especially when acute HF is imposed on chronic obstructive pulmonary disease (COPD) or chronic HF.
- Improve myocardial contractility/systemic perfusion.
- Reduce fluid volume overload.
- Prevent complications.
- Provide information about disease/prognosis, therapy needs, and prevention of recurrences.
- Assess Cardiovascular status including vital signs to detect cardiac compromise.
- Take an average of two or more blood pressure readings to establish hypertension.
- Check the client's blood pressure in lying, sitting, and standing position to determine if orthostatic hypotension is present. Also check for pallor, diaphoresis, and vertigo.
- Assess neurologic static and observe the client for changes that may indicated an alteration in cerebral perfussion (CVA or hemorrhage).
- Monitor and record intake and output and daily weight to detect fluid volume overload.
- Administer medications as prescribed to lower blood pressure.
- Make sure the client maintains a low-sodium, low-cholesterol diet to help minimize hypertention.
- Encourage the client to express feelings about daily stress to reduce anxity.
- Maintain a quiet environment to reduce stress.
- The client will exhibit a reduction in blood pressure
- The client will express understanding and acceptance of necessary lifestyle changes.
- Complications prevented/resolved.
- Optimum level of activity/functioning attained.
- Disease process/prognosis and therapeutic regimen understood.
- Plan in place to meet needs after discharge.
Labels: NCP Cardiovascular Disease
Read more...!
Management Nursing Care Plans @ 5:11 PM,
,
![]()
Nursing Care Plane For Anxiety
To decide what kind of nursing intervention or nursing management for the anxiety's patient, the Nurses should make an assessment in two point ; Actual or Potential before they make their nursing care plan (NCP) note. Then the nurses collect some information, why the patient become anxiety.
May be related to :
- Anesthesia intervention
- Anticipated or actual pain
- Him or Her condition (Disease)
- Invasive/noninvasive procedure during treatment
- Loss of significant other
- Threat to self-concept
- Other may appear on Him/Her self
To help and support the assessment's data, look and check on :
- Physiological; Elevated Blood Pressure , Pulls and Respiration. Insomnia, Restlessnes, Dry mouth, Dilated pupils, Frequent urination, Diarrhea.
- Emotional; Patient complains of apprehension, nervousness, tension
- Cognitive; Inability to concentrate. Orientation to past. Blocking of thoughts, hyper-attentiveness
Plan and Outcome data :
The patient will :
- Demonstrate a decrease in anxiety A.E.B.:
- A reduction in presenting physiological, emotional, and/or cognitive manifestations of anxiety.
- Verbalization of relief of anxiety.
- Discuss/demonstrate effective coping mechanisms for dealing with anxiety.
- Other:...
Nursing Interventions :
- Assist patient to reduce present level of anxiety by:
- Provide reassurance and comfort.
- Stay with person.
- Don't make demands or request any decisions.
- Speak slowly and calmly.
- Attend to physical symptoms. Describe symptoms: Give clear, concise explanations regarding impending procedures.
- Focus on present situation.
- Identify and reinforce coping strategies patient has used in the past.
- Discuss advantages and disadvantages of existing coping methods.
- Discuss alternate strategies for handling anxiety. (Eg.: exercise, relaxation techniques and exercises, stress management classes, directed conversation (by nurse), assertiveness training)
- Set limits on manipulation or irrational demands.
- Help establish short term goals that can be attained.
- Reinforce positive responses.
- Initiate health teaching and referrals as indicated:
- Other:...
Labels: NCP Psychology - Anxiety
Read more...!
Management Nursing Care Plans @ 12:18 AM,
,
![]()
Nursing Care Plan For Discharge Patient
When the doctor decided that the patient already in the good condition, The nurses have to prepare what they must do or see what is the patient needs after discharge from hospital.
Nursing care pan for the discharge patient do not important for the patient only, but to the family also the nurses should explain what they can do related to patient's needs.
Plan and Outcome data :
- The patient or family's discharge planning will begin on day of admission including preparation for the education and or equipment.
- On the day of discharge, patient / family will receive verbal and written instructions concerning: Medications, Diet, Activity, Treatments, Follow up appointments, Signs and symptoms to observe for (when to contact the doctor), Care of incisions, wounds, etc.
- Other data may can help.

Nursing Interventions :
- Assess needs of patient/family beginning on the day of admission and continue assessment during hospitalization.
- Anticipated needs/services:
- Respiratory equipment,
- Hospital bed,
- Wheel chair, Walker,
- Home health nurse,
- Home PT/OT/ST
- Involve the patient/family in the discharge process.
- Discuss with physician the discharge plan and obtain orders if needed.
- Contact appropraite personnel with orders.
- Provide written and verbal instructions at the patient/family's level of understanding.
- Verbally explain instructions to patient/family prior to discharge and provide patient/family with a written copy.
- Ascertain that patient has follow-up care arranged at discharge.
- Provide verbal and written information on what signs and symptoms to observe and when to contact the physician.
- Assess if any community resources should be utilized (i.e.: Home Health Nurse), and contact appropriate personnel.
- Document all discharge teaching on Discharge Instruction Sheet and Nursing notes.
- Other: ...
Labels: NCP Discharge Patient
Read more...!
Management Nursing Care Plans @ 11:42 PM,
,
![]()
Nursing Management
Nursing Management is the leading monthly source for practical, educational, cutting-edge information for nurse leaders. The Nursing management will perform a leadership functions of governance and decision-making within organizations employing nurses. A good nurse manager should be open to anything in the environment and be sensitive to the needs of the staff under her/his management.
In this website, we do not talking about some one who has profession as a Nurse manager. But we try to give many information what the nurses can do with his profession, especially how to manage health care delivery across the continuum of care.
In the other word, we write how the nurses make the Nursing Care Plan (NCP) and do the Nursing Intervention to the patient when they are admission, during treatment and discharge from hospital (Implementation of nursing care plan ).

Labels: Nursing Management
Read more...!
Management Nursing Care Plans @ 11:04 PM,
,
![]()
Nursing Care Plan
Nursing Care Plan (NCP) is an essential part of nursing practice that provides a written means of planning patient care and discharge planning based upon nursing diagnosis using some guide to meet the patient's needs.
Care planning provides a "road map" of sorts, to guide all who are involved with a patient or resident's care. The care plan has long been associated with nursing, and many people believe (inaccurately, in my opinion) that is the sole domain of nurses.
Nursing Care Plan is a set of actions from the nurses, They will implement care plan to resolve nursing problems which happened to the patient during treatment. The Nurses identified all of patient's problem by accurate and comprehensive assessment. The creation of the plan is an intermediate stage of the nursing process. It guides in the ongoing provision of nursing care and assists in the evaluation of that care.
To decided of Nursing Care Plan, For the first step the nurse collects subjective data and objective data, and then organizes the data into a systematic pattern as standard plans of care such as Marjory Gordon's functional health patterns. This step helps identify the areas in which the client needs nursing care.
Once the initial assessment is completed, a problem list should be generated. The nurse have to look at each problem and put the question "Can we make this problem better?" or "Can we keep this from getting any worse, or developing complications?".

After that, the nurse will put timing (review period) when the problem resolve or show signs of improvement. In the acute setting, the review period may be as short as next shift, next day or next week. In the long-term or home health setting, the review period will likely be longer.
When the problem is not getting better or not likely to improve, and deterioration is inevitable, then the nurse will decided last question "What can we do to provide optimal quality of life, comfort and dignity for this person?"
To make a better Nursing Care Plan, the Nurses must follow the steps of the nursing process bellow :
- Assessment (collect data from medical record, do a physical assessment of the patient, assess ADL's, look up information about your patient's medical diseases/conditions to learn about the signs and symptoms and pathophysiology)
- Determination of the patient's problem(s)/Nursing diagnosis (make a list of the abnormal assessment data, match your abnormal assessment data to likely nursing diagnoses, decide on the nursing diagnoses to use)
- Planning (write measurable goals/outcomes and nursing interventions)
- Implementation (initiate the care plan)
- Evaluation (determine if goals/outcomes have been met)
Labels: Nursing Care Plan
Read more...!
Management Nursing Care Plans @ 12:38 AM,
,
![]()










